Dental-General
Dental Topics

Oral Hygiene
Flossing
For areas between the teeth that a toothbrush can’t reach, dental floss is used to remove food particles and plaque. Dental floss is a thin thread of waxed nylon that is used to reach below the gum line and clean between teeth. It is very important to floss between your teeth every day.
Pull a small length of floss from the dispenser. Wrap the ends of the floss tightly around your middle fingers. Guide the floss between all teeth to the gum line, pulling out any food particles or plaque. Unwrap clean floss from around your fingers as you go, so that you have used the floss from beginning to end when you finish. Floss behind all of your back teeth.
Floss at night to make sure your teeth are squeaky clean before you go to bed. When you first begin flossing, your gums may bleed a little. If the bleeding does not go away after the first few times, let us know at your next appointment.
Brushing
Use a toothbrush with soft bristles and a small strip of fluoride toothpaste. When you brush your teeth, move the brush in small circular motions to reach food particles that may be under your gum line. Hold the toothbrush at an angle and brush slowly and carefully, covering all areas between teeth and the surface of each tooth. It will take you several minutes to thoroughly brush your teeth. Brush up on the lower teeth, down on the upper teeth and the outside, inside and chewing surface of all of your front and back teeth. Brush your tongue and the roof of your mouth before you rinse.
Brush your teeth four times daily to avoid the accumulation of food particles and plaque:
In the morning after breakfast
After lunch or right after school
After dinner
At bedtime
As soon as the bristles start to wear down or fray, replace your toothbrush with a new one. Do not swallow any toothpaste, rinse your mouth thoroughly with water after you finish brushing. It is important to carefully floss and brush daily for optimal oral hygiene.

About Your Teeth
About Your Teeth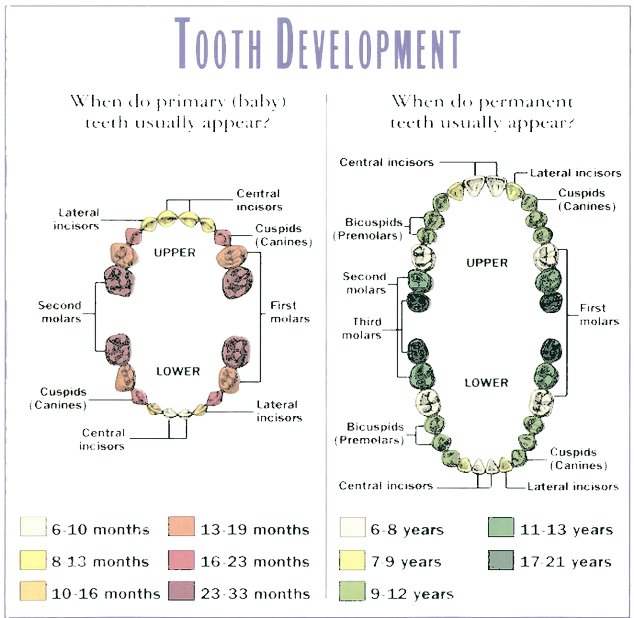
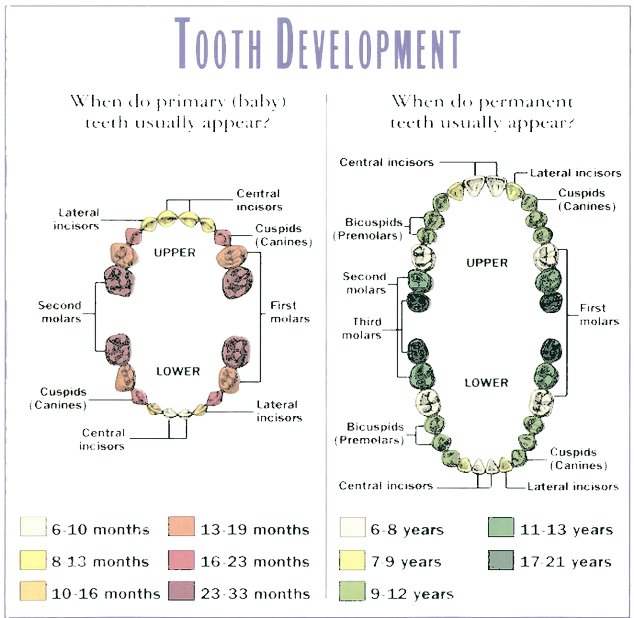
Throughout your life, you will have two sets of teeth: primary (baby) teeth and secondary (permanent) teeth. At age 6-8 months, the primary teeth appear; all 20 are in place by age 3.
Permanent teeth will begin to grow around age 6, and except for wisdom teeth, are all present between ages 12 and 14. The next teeth to grow in are the 12-year molars and finally the wisdom teeth. Wisdom teeth typically begin breaking through from age 17 and on. The total number of permanent teeth is 32, though few people have room for all 32 teeth. This is why wisdom teeth are usually removed.
Your front teeth are called incisors. The sharp “fang-like” teeth are canines. The next side teeth are referred to as pre-molars or bicuspids, and the back teeth are molars. Your permanent teeth are the ones you keep for life, so it is vital that they are brushed and flossed regularly and that periodic check-ups by a dentist are followed.
Dental Health
Dental Health
Studies and research have concluded on the importance of starting children early in their lives with good dental hygiene and oral care. According to research, the most common chronic childhood disease is tooth decay, affecting 50 percent of first-graders and 80 percent of 17-year-olds. Early treatment prevents problems affecting a child’s health, well-being, self-image and overall achievement.
Research estimates that children will miss 52 million hours of school each year due to oral health problems and about 12.5 million days of restricted activity every year from dental symptoms. Because there is such a significant loss in their academic performance, the Surgeon General has made children’s oral health a priority.
Parents are responsible for ensuring their children practice good dental hygiene. Parents must introduce proper oral care early in a child's life—as early as infancy. good oral hygiene routine for children includes:
- Thoroughly cleaning your infant’s gums after each feeding with a water-
soaked infant cloth. This stimulates the gum tissue and removes food. - Gently brushing your baby’s erupted teeth with a small, soft-
bristled toothbrush and using a pea- sized amount of fluoridated toothpaste. - Teaching your child at age 2 or 3 about proper brushing techniques and later teaching them brushing and gentle flossing until 7 or 8 years old.
- Regular visits with their dentist to check for cavities in the primary teeth and for possible developmental problems.
- Encouraging your child to discuss any fears they may have about oral health visits, but not mentioning words like “pain” or “hurt,” since this may instill the possibility of pain in the child’s thought process.
- Determining if the water supply that serves your home is fluoridated, if not, discussing supplement options with your dentist or hygienist.
- Asking your hygienist or dentist about sealant applications to protect your child’s teeth-
chewing surfaces and about bottle tooth decay, which occurs when teeth are frequently exposed to sugared liquids.
Early Dental Care
Early Dental Care
Our goal for children under 3 is to make dental visits quick and easy. We will provide a thorough examination and talk with you about any issues while your child plays nearby. With each subsequent visit your child will mature and confidence and trust will most likely increase.
Infant Tooth Eruption
A child’s teeth actually start forming before birth. As early as 4 months of age, the primary or “baby” teeth push through the gums—the lower central incisors are first, then the upper central incisors. The remainder of the 20 primary teeth typically erupt by age 3, but the place and order varies.
Permanent teeth begin eruption around age 6, starting with the first molars and lower central incisors. This process continues until around age 21. Adults have 28 secondary (permanent) teeth—32 including the third molars (wisdom teeth).
Preventing Baby Bottle Tooth Decay
Tooth decay in infants can be minimized or totally prevented by not allowing sleeping infants to breast or bottle-feed. Infants that need a bottle to comfortably fall asleep should be given a water-filled bottle or a pacifier. Let us know if you notice any signs of decay or anything unusual in your child’s mouth.
Teething
Normally the first tooth erupts between ages 6 to 12 months. Gums are sore, tender and sometimes irritable until the age of 3. Rubbing sore gums gently with a clean finger, the back of a cold spoon or a cold, wet cloth helps soothe the gums. Teething rings work well, but avoid teething biscuits—they contain sugar that is not good for baby teeth.
While your baby is teething, it is important to monitor the teeth for signs of baby bottle decay. Examine the teeth, especially on the inside or the tongue side, every two weeks for dull spots (whiter than the tooth surface) or lines. A bottle containing anything other than water and left in an infant’s mouth while sleeping can cause decay. This happens because sugar in the liquid mixes with bacteria in dental plaque, forming acids that attack the tooth enamel. Each time a child drinks liquids containing sugar, acids attack the teeth for about 20 minutes. When awake, saliva carries away the liquid. During sleep, the saliva flow significantly decreases and liquids pool around the child’s teeth for long periods, covering the teeth in acids. surface) or lines. A bottle containing anything other than water and left in an infant’s mouth while sleeping can cause decay. This happens because sugar in the liquid mixes with bacteria in dental plaque, forming acids that attack the tooth enamel. Each time a child drinks liquids containing sugar, acids attack the teeth for about 20 minutes. When awake, saliva carries away the liquid. During sleep, the saliva flow significantly decreases and liquids pool around the child’s teeth for long periods, covering the teeth in acids.

Common Problems
Cavities and Tooth Decay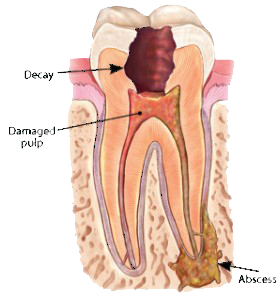
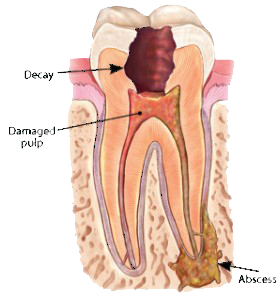
Caries, or tooth decay, is a preventable disease. While caries might not endanger your life, they may negatively impact your quality of life.
When your teeth and gums are consistently exposed to large amounts of starches and sugars, acids may form that begin to eat away at tooth enamel. Carbohydrate-rich foods such as candy, cookies, soft drinks and even fruit juices leave deposits on your teeth. Those deposits bond with the bacteria that normally survive in your mouth and form plaque. The combination of deposits and plaque forms acids that can damage the mineral structure of teeth, with tooth decay resulting.
Plaque is a film of bacteria that forms on teeth and gums after eating foods that produce acids. These foods may include carbohydrates (starches and sugars), such as candy and cookies, and starchy foods, such as bread, crackers, and cereal.
Tooth decay leads to cavities and occurs when plaque remains on your teeth for an extended period of time, allowing the bacteria to "eat away" at the surfaces of your teeth and gums. Ironically, the areas surrounding restored portions of teeth (where fillings, or amalgams have been placed) are particularly vulnerable to decay and are a breeding ground for bacteria.
In addition to causing cavities, plaque can lead to gum irritation, soreness, and redness. Sometimes, your gums may begin to bleed as a result of plaque accumulation. Long-term, plaque can lead to serious problems. Sometimes, the bacteria can form pockets of disease around tooth structures, eventually destroying the bone beneath the tooth.
In regards to early childhood caries, avoid putting your baby or small child to sleep with a bottle containing anything but water, because juices and milk contain sugars that can be harmful to teeth. When a child sleeps, these liquids "pool" in the mouth and bathe the teeth.
Early childhood caries may occur when sweetened liquids, such as milk, formula, and fruit juice, are given and are left to pool in an infant's mouth for long periods of time. Baby bottle tooth decay can lead to severe cavities in your child's mouth, and destroy the teeth if left untreated.
Avoid allowing your child to fall asleep with a bottle and avoid breast feeding at will after the first baby tooth begins to erupt.
Jaw disorders/TMD(temporomandibular disorders)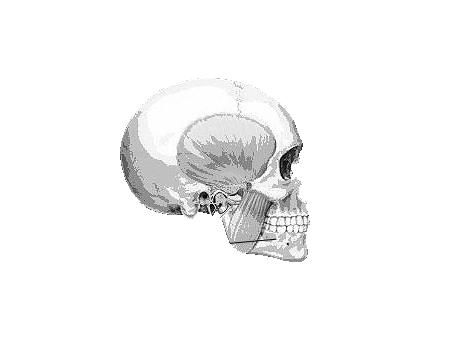
The temporomandibular joint (TMJ) connects the lower jaw, called the mandible, to the temporal bone at the side of the head. Because these joints are flexible, the jaw can move smoothly up and down and side to side, enabling us to talk, chew and yawn. Muscles attached to and surrounding the jaw joint control its position and movement.
When we open our mouths, condyles, or the rounded ends of the lower jaw, glide effortlessly along the joint socket of the temporal bone. A soft disc lies between the condyle and the temporal bone to ensure smooth motion. This disc absorbs shocks to the temporomandibular joint from chewing and other movements.
Temporomandibular (jaw) disorders, also called "TMD" or "TMJ syndrome," are a general class of health problems associated with the jaw. TMD may occur when the jaw twists during opening, closing, or side-motion movements. These movements affect the jaw joint and the muscles that control chewing.
TMD is not just one disorder, but a group of conditions, often painful, that affect the jaw joint (temporomandibular joint, or TMJ) and the muscles that control chewing. Although researchers don't yet know how many people actually have TMD, the disorders appear to affect about twice as many women as men, according to the National Institute of Dental and Craniofacial Research.
Teeth Grinding (bruxism) & Orthodontic Problems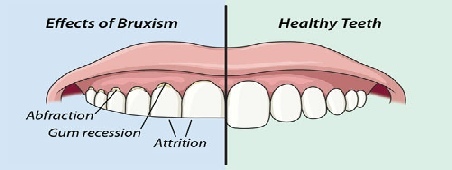
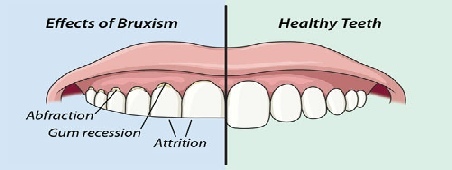
Teeth grinding (also called bruxism) is often viewed as a harmless, though annoying habit. Some people develop bruxism from an inability to deal with stress or anxiety.
However, teeth grinding can literally transform your bite relationship and worse, severely damage your teeth and jaws over long periods of time.
Teeth grinding can cause abrasion to the chewing surfaces of your teeth.
This abnormal wear and tear will prematurely age and loosen your teeth, and open them to problems such as hypersensitivity (from the small cracks that form, exposing your dentin.) Bruxism can also lead to chronic jaw and facial pain, as well as headaches.
loosen your teeth, and open them to problems such as hypersensitivity (from the small cracks that form, exposing your dentin.) Bruxism can also lead to chronic jaw and facial pain, as well as headaches.
 loosen your teeth, and open them to problems such as hypersensitivity (from the small cracks that form, exposing your dentin.) Bruxism can also lead to chronic jaw and facial pain, as well as headaches.
loosen your teeth, and open them to problems such as hypersensitivity (from the small cracks that form, exposing your dentin.) Bruxism can also lead to chronic jaw and facial pain, as well as headaches.If no one has told you that you grind your teeth, here are a few clues that you may suffer from bruxism:
● Your jaw is often sore, or you hear popping sounds when you open and close your mouth.
● Your teeth look abnormally short or worn down.
● You notice small dents in your tongue.
Bruxism is somewhat treatable. A common therapy involves use of a special appliance worn while sleeping. Less intrusive, though just as effective methods could involve biofeedback, and behavior modification methods such as tongue exercises and learning how to properly align your tongue, teeth and lips.
Sensitive Teeth & Bad Breath (Halitosis)
Your teeth expand and contract in reaction to changes in temperature. Hot and cold food and beverages can cause pain or irritation to people with sensitive teeth. Over time, tooth enamel can be worn down, gums may recede or teeth may develop microscopic cracks, exposing the interior of the tooth and irritating nerve endings. Just breathing cold air can be painful for those with extremely sensitive teeth.
Bad Breath (Halitosis)
Daily brushing and flossing helps to prevent the buildup of food particles, plaque and bacteria in your mouth. Food particles left in the mouth deteriorate and cause bad breath. While certain foods, such as garlic or anchovies, may create temporary bad breath, consistent bad breath may be a sign of gum disease or another dental problem.
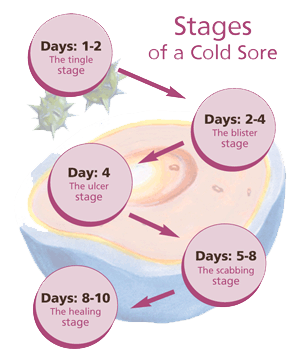
Canker Sores / Cold Sores

Canker sores (also called recurrent aphthous ulcers, or RAU) and cold sores are not the same thing. Canker sores occur inside the mouth, and cold sores usually occur outside the mouth, usually on or near the lips.
A canker sore is a small ulcer with a white or gray base and red border. There can be one or a number of sores in the mouth. Canker sores are very common and recur often, but their cause is unknown.
A cold sore, which is also called fever blister and is caused by the "herpes simplex" virus, is composed of groups of painful, fluid-filled blisters that often erupt around the lips and sometime under the nose or under the chin. Cold sores are usually caused by herpes virus type I and are very contagious.
Canker sores, like all ulcers, are very difficult to treat.
There is no proven technique that will eliminate ulcers or speed the recovery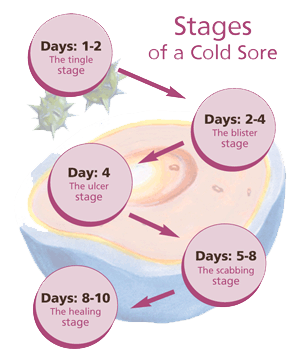 time once they appear.
time once they appear.
 time once they appear.
time once they appear. There are a few medications that will give temporary relief from the pain, but they need to be started as soon as symptoms appear.
Canker sores usually heal in about a week or two. Over-the-counter topical anesthetics can also provide relief.
Cold sores usually heal in about a week. Over-the-counter topical anesthetics can provide temporary relief, and prescription antiviral drugs may reduce these kinds of viral infections.
Sore gums. teething, pacifiers & thumb sucking
When babies are teething, usually between the ages of four months and 2.5 years, they often have sore and tender gums. The pain usually can be soothed by gently rubbing the baby's gums with a clean finger, a small, cool spoon or a wet gauze. A clean teething ring for the baby to chew on also may be helpful.
Pacifiers & thumb sucking
In general, I would discourage thumb sucking or pacifiers after the age of 4 because they may lead to overcrowded and crooked teeth, as well as bite problems. In some cases, the upper front teeth may tip toward the lip or not come in properly if thumb, finger, or pacifier sucking continues after the age of 4.
From six months to age 3, your child may have sore gums when her teeth erupt. Many parents use a clean teething ring, a cool spoon, or a cold wet washcloth. You also can rub the baby's gums with a clean finger.
A mouth appliance may be effective on children if they are still sucking their thumbs or fingers when the permanent teeth arrive.
Gingivitis / Gum Disease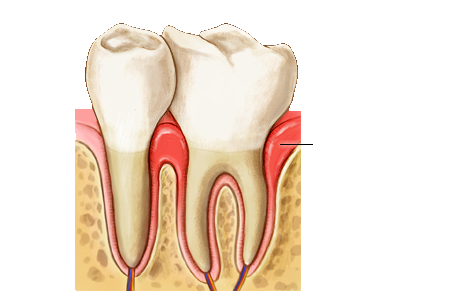
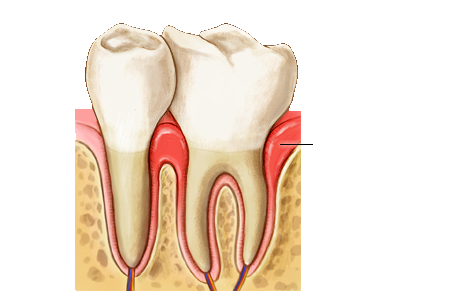
Periodontal disease is a condition in which the structures that support the teeth, including the gums and bone surrounding each tooth, become infected and begin to break down. Periodontal disease (also known as "periodontitis") can be influenced by the body's response to infection caused by the bacteria in plaque. Poor oral hygiene in children could set the stage later on for gum disease - the major cause of tooth loss in adults. It is most often caused by bacteria.
In the early stage of gum disease, called gingivitis, the gums can become red, swollen and easily bleed. At this stage, the disease is still reversible and can usually be eliminated by daily brushing and flossing.
Like some diseases, gum disease isn't painful until it reaches a more critical stage, in which treatment options narrow.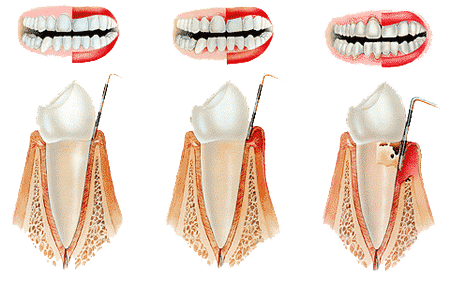
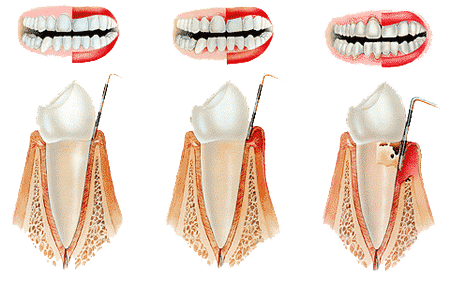
If it goes unchecked, inflammation begins to allow surrounding bone to demineralize and dissolve. As the bone dissolves around the teeth in the more advanced stages of gum disease, called periodontitis, the gums and bone that support the teeth can become seriously damaged. The teeth can become loose, fall out, or have to be removed.
Early symptoms of gum disease
● Gums that bleed when you brush your teeth
● Red, swollen or tender gums
● Gums that have pulled away from the teeth
● Persistent bad breath
● Pus between your teeth and gums
● Loose teeth
● A change in the way your teeth fit together when you bite
Bulimia Nervosa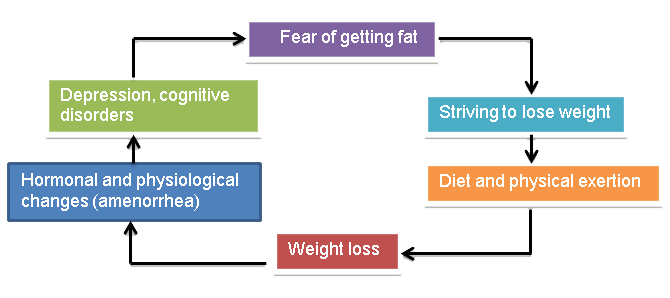
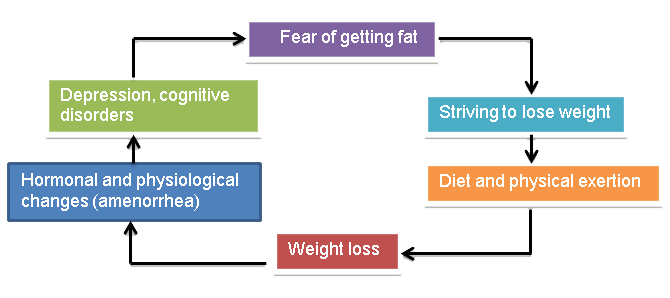
Typically, patients who suffer from bulimia nervosa have small, purplish-red lesions on their palate due to contact with objects used to induce vomiting. Silver fillings often become raised due to erosion of the teeth, and braces and temporary restorations may not stay on the teeth because the acid will dissolve the temporary cement used to keep these materials in place. Teeth may be discolored or look dull from the acid.
Avoid brushing teeth after vomiting, and rinse with water instead. Use a basic rinse, such as baking soda and water; immediately after vomiting to neutralize the acid. Remove plaque by brushing and flossing properly. Chew sugarless gum to increase salivary flow or use artificial saliva. Use fluoride either in toothpastes, rinses or gels to reduce sensitivity of teeth and build resistance to decay from acid.
Impacted Teeth / Wisdom Teeth

Your child's third set of molars are no different than any other tooth, save for the fact that they are the last to erupt, or grow, into the mouth. Because they typically do so at around the age of 18 to 20, when adolescents are close to turning into adults, these teeth are commonly referred to as "wisdom teeth."
People normally have three permanent molars that develop in each quadrant of the mouth - upper, lower, right, and left. The first molars usually grow into the mouth at around six years of age. The second molars grow in at around age 12.
In many cases, wisdom teeth do not grow in properly, have a proper bite relationship, or have unhealthy gum tissue around them. Often, wisdom teeth improperly erupt or become impacted, requiring them to be extracted.
usually in the adolescent years.
 Our office must examine your child's mouth and X-rays to determine if the teeth are impacted or will not grow in properly. Impacted teeth may cause problems that can lead to infection, adjacent tooth resorption, gum disease, cysts, or tumors.
Our office must examine your child's mouth and X-rays to determine if the teeth are impacted or will not grow in properly. Impacted teeth may cause problems that can lead to infection, adjacent tooth resorption, gum disease, cysts, or tumors.To avoid potential problems later in life, many dentists safely remove impacted wisdom teeth. Although they are like any other teeth, most people continue to have normal bites and well functioning sets of teeth in their absence.
Symptoms of impacted teeth
● Pain
● Infection in the mouth
● Facial swelling
● Swelling of the gum line in the back of the mouth
● Wisdom teeth are typically removed after the roots are formed, or at least three-fourths developed.

Emergency
Bitten Lip or Tongue or Cheek
Ice can be applied to any bruised areas. For bleeding, apply firm (but gentle) pressure with sterile gauze or a clean cloth. If the bleeding does not stop with pressure or continues after 15 minutes, go to an emergency room.
Tooth Ache
It is important to get an evaluation from one of our dentists as soon as possible if your child has intra-oral pain. Please call our office ahead of time so we may reserve the most efficient appointment time for you. If ignored, dental pain may lead to larger problems in some cases.
If your child has a toothache, rinse the irritated area with warm salt water. Gently use dental floss or an inter-dental cleaner to ensure that there is no food or other debris caught between your child's teeth. Place a cold compress on the face if it is swollen.
UNDER NO CIRCUMSTANCES should you use aspirin on the aching tooth or on the gum
Broken or Problems with Braces and Retainers
Remove a broken appliance only if it comes out easily. If it is lodged or painful to remove, cover any protruding edges with wax, cotton balls, gauze or chewing gum. DO NOT REMOVE any wire caught in the gums, cheek or tongue; see a dentist immediately. Emergency attention is usually not required for loose or broken appliances that cause no discomfort.
Broken wires and braces
If a wire is causing irritation, cover the end with a small cotton ball, beeswax or a piece of gauze until you can get to the dentist. If a wire gets stuck in the cheek, tongue or gum tissue, do not attempt to remove it. Contact our office. If an appliance becomes loose or a piece of it breaks off, collect the broken appliance or piece and contact our office immediately.
Trapped Debris/Objects Between Teeth
Try gently removing the debris with dental floss. Be careful not to cut your child's gums. Never use a sharp instrument, such as a needle or pin, to remove any object that is stuck between teeth. If you can't dislodge the object using dental floss, contact our clinic.
Broken, Fractured, Displaced Tooth
Rinse the area with warm water. Put a cold compress over the facial area of the injury. Recover any broken tooth fragments. Get immediate dental attention.
Knocked out permanent tooth
Recover the tooth, making sure to hold it by the crown (top) and not the root end. Rinse, but do not clean or handle the tooth more than necessary. Reinsert the tooth in the socket and hold it in place using a clean piece of gauze or cloth. If the tooth cannot be reinserted, carry it in a cup containing milk or water. Because time is essential, see a dentist immediately.
Sports Injuries
What do the following have in common?
A bat…….A ball……..A knee or elbow…..A hard surface, such as the ground or the bottom of a swimming pool.
They all are things that could easily come into contact with your child's mouth when participating in sports. And they all have the potential for damaging or knocking out teeth, or fracturing or dislocating a jaw. High-risk activities include "contact" sports, such as football, boxing, martial arts (including karate and kick-boxing) and hockey, as well as non-contact sports such as basketball, baseball, bicycle riding, roller-blading, soccer, wrestling, racquetball, surfing, and skateboarding.
A bat…….A ball……..A knee or elbow…..A hard surface, such as the ground or the bottom of a swimming pool.
They all are things that could easily come into contact with your child's mouth when participating in sports. And they all have the potential for damaging or knocking out teeth, or fracturing or dislocating a jaw. High-
Even swimming, with all of its gentility, poses serious hazards for your child's teeth. Common swimming pool accidents occur when children, swimming underwater, quickly ascend to the surface, hitting the hard ledge, and loosening the front tooth. Running on slippery, slick cement and ceramic pool surfaces also can send your child headfirst into the ground, increasing the likelihood of a chipped or loose tooth.
If your child participates in any sports, a mouth guard is a smart investment. Mouth guards are soft plastic devices that fit over the front of your child's mouth, protecting his teeth, lips, cheeks, and gums from sports-related injuries. A well-fitting mouth guard can protect your child from injuries to the teeth, face, and even some severe injuries to the head.
Other Emergency Conditions
Possible Broken Jaw
In the event of jaw injury, tie the mouth closed with a towel, tie or handkerchief. Go immediately to an emergency room.
Bleeding After a Baby Tooth Falls Out
Fold a piece of gauze and place it (tightly) over the bleeding area. Bite down on the gauze for 15 minutes; if bleeding continues, see a dentist.
Cold or Canker Sores
Over-the-counter medications will usually provide temporary relief. If sores persist, visit your dentist.

Prevention
Prevention
Tooth Decay Prevention
Tooth decay is a progressive disease resulting in the interaction of bacteria that naturally occur on the teeth and sugars in the everyday diet. Sugar causes a reaction in the bacteria, causing it to produce acids that break down the mineral in teeth, forming a cavity. Dentists remove the decay and fill the tooth using a variety of fillings, restoring the tooth to a healthy state. Nerve damage can result from severe decay and may require a crown (a crown is like a large filling that can cap a tooth, making it stronger or covering it). Avoiding unnecessary decay simply requires strict adherence to a dental hygiene regimen: brushing and flossing twice a day, regular dental checkups, diet control and fluoride treatment. Practicing good hygiene avoids unhealthy teeth and costly treatment.
Sealants
The grooves and depressions that form the chewing surfaces of the back teeth are extremely difficult (if not impossible) to clean of bacteria and food. As the bacteria reacts with the food, acids form and break down the tooth enamel, causing cavities. Recent studies indicate that 88 percent of total cavities in American school children are caused this way.
Tooth sealants protect these susceptible areas by sealing the grooves and depressions, preventing bacteria and food particles from residing in these areas. Sealant material is a resin typically applied to the back teeth, molars and premolars and areas prone to cavities. It lasts for several years but needs to be checked during regular appointments.
Fluride
Fluoride is a substance that helps teeth become stronger and resistant to decay. Regularly drinking water treated with fluoride and brushing and flossing regularly ensures significantly lower cavities. Dentists can evaluate the level of fluoride in a primary drinking water source and recommend fluoride supplements (usually in tablets or drops), if necessary.
Thumb Sucking
Sucking is a natural reflex that relaxes and comforts babies and toddlers. Children usually cease thumb sucking when the permanent front teeth are ready to erupt. Typically, children stop between the ages of 2 and 4 years. Thumb sucking that persists beyond the eruption of primary teeth can cause improper growth of the mouth and misalignment of the teeth. If you notice prolonged and/or vigorous thumb sucking behavior in your child, talk to your dentist.
Here are some ways to help your child outgrow thumb sucking:
Don’t scold a child when they exhibit thumb sucking behavior; instead, praise them when they don’t thumb suck.
Focus on eliminating the cause of anxiety—thumb sucking is a comfort device that helps children cope with stress or discomfort.
Praise them when they refrain from the habit during difficult periods.
Place a bandage on the thumb or a sock on their hand at night.

Dental Anesthesia
Dental Anesthesia
General anesthesia is commonly used to facilitate dental treatment in patients with anxiety or challenging behavior, many of whom are children or patients with special needs.
When performing procedures under general anesthesia, dental surgeons must perform a thorough pre-operative assessment.
Such precautions ensure optimal patient management and reduce the frequency of morbidities associated with this form of sedation.
The field encompasses a wide variety of patients, including those with intellectual disabilities, physical impairments, psychiatric problems, and complex medical backgrounds. In many cases, these conditions can have significant effects on oral health. Additionally, they often influence the manner in which patients receive oral healthcare. Part of the role of the special needs dentist is to adapt dental treatment to the individual needs of the patient. In many situations, this may necessitate pharmacological sedation, ranging from minimal sedationachieved through oral, transmucosal, or inhalation sedation—to deeper forms of sedation and general anesthesia.

Distraction Techniques
Distracting Pediatric Patients During Procedures
Techniques are chosen based on both the child's age and developmental stage, which may differ from the child's chronologic age. Developmentally appropriate techniques help divert the child's focus from potentially painful procedures such as laceration repair or dressing changes.
Examples of age-appropriate distraction techniques include the following.
* Infants respond well to the soothing effect of swaddling because it helps to satisfy an infant's developmental need to be held.
* Safe and effective distraction techniques for toddlers can be as simple as blowing bubbles or playing peek-a-boo.1
* School-aged children and adolescents may respond well to audiovisual distractions,

Nursing Bottle Mouth Syndrome
Nursing Bottle Mouth Syndrome
Also known as early childhood caries, baby bottle tooth decay refers to tooth decay in infants and toddlers. Your child needs strong, healthy primary teeth to properly chew food and learn to speak, so preventing baby bottle tooth decay is very important.
The Causes of Tooth Decay in Children
There are many risk factors when it comes to children’s tooth decay. A common cause is the frequent and prolonged exposure of your child’s teeth to sugary drinks, including milk, formula, and fruit juice. Giving you child a sugary drink at nap or night-time can be especially harmful, because the flow of saliva decreases during sleep. Bacteria in the mouth thrive on sugar and produce acids that attack the teeth.
Tooth decay can also be caused by bacteria passed from you to your baby through saliva by sharing spoons, testing foods before feeding them to your baby, and cleaning off a pacifier in your mouth instead of with water. These germs can start the process that causes cavities even before your baby’s primary teeth emerge, so it’s important to avoid sharing saliva with your baby from the start.
If your infant or toddler does not receive an adequate amount of fluoride internally through water, especially if he or she drinks bottled water, there can also be an increased risk for tooth decay. Your pediatric dentist may prescribe fluoride supplements to help prevent tooth decay.
Tooth Decay Prevention
The good news about baby bottle tooth decay is that it’s preventable!
- Wipe your baby’s gums with a clean gauze pad or washcloth after each feeding.
- Begin brushing your child’s teeth, without toothpaste, when the first tooth comes in.
- Clean and massage gums in areas without teeth.
- Place only formula, milk, or breast milk in bottles. Avoid filling a bottle with liquids like sugar water, juice, or soft drinks.
- Never allow your child to fall asleep with a bottle that contains anything but water.
- Never dip a pacifier in anything sweet, like sugar water or honey.
- Schedule an appointment with your pediatric dentist by your child’s first birthday or when the first teeth begin to emerge.
Remember, healthy little smiles grow up to be healthy big smiles!

Rampant Caries
Rampant Caries
Adolescent rampant caries is a new and growing challenge in Conservative Dentistry. It has the same etiology and pattern as that of nursing bottle syndrome. Herein, a case is presented in which the main cause of rampant caries is the patient's habit of keeping cariogenic food in her mouth and going to sleep. Educating this etiology and introduction of preventive strategies not only assists in meeting the special oral needs of the adolescent population, but also helps to establish lifelong healthful habits.
Rampant caries is of the following three types :
- Nursing bottle rampant caries.
- Adolescent rampant caries.
- Xerostomia-induced rampant caries.
Nursing bottle rampant caries is very common in infants.
Adolescent rampant caries ;
When rampant caries occurs in adolescent age, it is called adolescent rampant caries. During adolescence, some children habitually put chocolates, toffees and biscuits in their mouth and go to sleep.[1] Such patients suffer from adolescent rampant caries. The adolescent rampant caries has the same pattern as that of nursing bottle caries.
Xerostomia-induced rampant caries :
Is often associated with salivary gland hypofunction due to irradiation of the head and neck region.

Educational Videos
About Teeth for Kids
Proper Tooth Brushing
Teeth Grinding
What is a Cavity?
How to floss your teeth